Among all the ailments the human body may face, cancer is one of the trickiest. It can grow stealthily, evade detection, evolve complex defenses to drugs. Researchers have been studying cancer, and developing drugs to fight it, for decades in hopes of one day stamping out the mutant cells that are constantly outsmarting our immune systems.
It is urgent work. According to the U.S. National Cancer Institute, more than one third of all men and women will be diagnosed with cancer at some point during their lifetimes. The disease kills millions worldwide every year, and the number of new cancer cases annually continues to rise, projected to reach 23.6 million by 2030.
In this epic health batle, many scientists are turning to high magnetic fields as their weapons of choice, using magnetic resonance imaging (MRI) and other magnet-based techniques. Today, stronger magnets, clearer images, better data resolution and novel techniques are leading to new cancer discoveries on everything from brain tumors to pancreatic cancer to multiple myeloma. At the National High Magnetic Field Laboratory (National MagLab) in Tallahassee, Florida, and similar labs worldwide, scientists are pushing the boundaries of cutting-edge instruments to learn how to better detect, treat and track this deadly disease.
Detect Early
Cancers often develop undetected. By the time a patient starts to experience symptoms, it might be too late to treat. Researchers are looking at how high-field tools could help.
Cancers often develop undetected. By the time a patient starts to experience symptoms and goes to a doctor, it could be too late. Researchers are looking at ways high-field tools could help.
At the National MagLab, analytical chemist Lissa Anderson is collaborating with researchers from the Mayo Clinic in Rochester, Minnesota, to detect multiple myeloma early. Multiple myeloma is a cancer of immune cells called B cells, which mature into plasma cells that produce antibodies (immunoglobulins) that help the body defend against foreign invaders. But when these cells turn cancerous, they proliferate and secrete too many antibodies.
Doctors currently use a technique called gel electrophoresis to detect these excess antibodies (and by extension multiple myeloma). But this approach can't identify the exact antibodies being overexpressed. Clinicians can determine this by genome sequencing, but that process requires a bone marrow biopsy, which can be costly, painful and inaccurate.
"False negative are possible because you might not be sampling in an area where there's an abundance of these transformed B cells," Anderson said.
Anderson and her colleagues have used the world's most powerful ion cyclotron resonance (ICR) mass spectrometer to overcome the limitations of conventional methods. Thanks to its 21-tesla magnet, the instrument can sequence these overexpressed antibodies. This allows researchers to stratify patients into different categories depending upon which antibodies are being overexpressed, allowing for precision diagnosis and personalized treatment. The methods being developed could help in the early detection and monitoring of multiple myeloma. In fact, the sensitivity of their measurements is 10 times higher than what doctors now get in clinical testing, Anderson said, and a simple blood draw is all that is required.
"With this approach, it's possible to track the progression of the disease as we see the cells undergo further transformation because of the cancer — the sequences of these antibodies are always undergoing mutations," Anderson said. "As the disease progresses, we can track the mutation status of the antibodies and the number of single amino acid substitutions that are happening. No one has ever even done that, to my knowledge."
It's important to find out early when cancer first strikes. But it's equally critical to detect when a cancer doctors hoped was vanquished makes a comeback. Because of the very high sensitivity of this instrument, Anderson said, it could be used to identify a relapse well before symptoms resurface.
"That hasn't been done, yet," she said, "but what we have demonstrated is that that could be done."
Claudio Luchinat, a chemist at the University of Florence in Italy, is using another spectroscopic technique, nuclear magnetic resonance (NMR), to detect relapses of the most common kind of cancer: breast cancer.
Mammography detects tumors about a centimeter in size or larger, but is useless when tumors are tinier. Luchinat, however, has discovered that new tumors produce another telltale clue: They affect the metabolites of the host, changes that are detectable in blood.
"It seems miraculous that you can tell the presence of a very tiny metastasis by looking at something that seems unrelated," said Luchinat.
When Luchinat took samples of serum from early breast cancer patients and analyzed them using a 600 MHz/14.1-tesla NMR magnet, he found that the set of metabolites in women who, after treatment, remained free from the disease differed from those who eventually relapsed. In fact, Luchinat discovered that the "metabolic fingerprint" was accurate about 80% of the time in predicting if a patient will relapse.
In order to demonstrate the applicability of the technique to clinical practice, Luchinat is broadening his research to see if the fingerprint works within different populations. He is also studying whether other cancers generate a similar fingerprint.


Lissa Anderson

Claudio Luchinat
Treat Agressively
Once cancer has been spotted, the next step is, of course, to stamp it out. With high magnetic fields, researchers are trying to improve the aim of anti-cancer drugs.
In the last few years, T-cell therapies have emerged as a promising form of cancer treatment. But many questions remain about how they work and how to improve them.
Likai Song, a biophysicist and medical doctor at the National MagLab, is tackling that question by collaborating with researchers at the Dana Farber Cancer Institute in Boston. Together, they study how T-cells, frontline defenders of our immune system, get activated.
For this work, Song and his colleagues paired a technique called electron magnetic resonance (EMR) with NMR. (While NMR targets atoms’ nuclei to identify the structure of molecules, EMR gleans information from the electrons.) With this dynamic magnet duo, they study how proteins on the surface of T-cells react to their environment, thereby triggering the T-cell to attack. The team has determined the molecular structure of parts of the protein and observed how that structure changes when T-cells are activated. Knowing these specific shapes, Song said, will help scientists to design new therapies, such as small-molecule drugs with a complementary structure that fits these sites like a set of keys. Doctors could then fine-tune the T-cell response, amping it up or dialing it back to fit the specific requirements of individual patients.
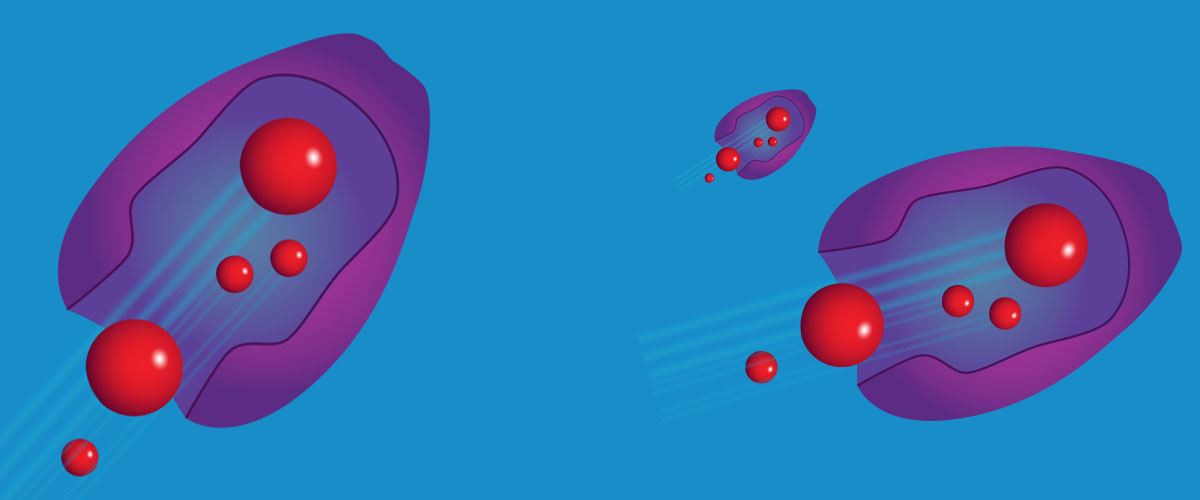
But even the best cancer drug is useless if it never hits the bull’s-eye. That’s why Edward Agyare, an associate professor of pharmaceutics at Florida A&M University in Tallahassee, has been testing a way to verify that drugs intended to zap pancreatic cancer reach their target.
Pancreatic cancer has the lowest five-year survival rate of any leading cancer and is projected to become the second leading cause of cancer-related deaths in the United States next year. These tumors are challenging to treat because they’re surrounded by a lot of dense, fibrous tissue.
Agyare is trying to get around this defense by developing nanoparticles with a one-two punch. They contain both gemcitabine, a drug used to treat the cancer, and gadolinium, a contrast agent that researchers can track in the body using MRI. These nanoparticles are also coated with a protein designed to bind to tumor cells.
Contrast agents are typically metabolized by an animal's system; packaging them into the same vehicle used to deliver drugs could one day help doctors verify if those drugs make it all the way to their destination. Agyare has been testing this approach in animal models using the National MagLab's 21.1-tesla MRI machine, the strongest MRI machine used for small animal research in the world.
Part of this research, which Agyare conducts with collaborators at the University of Florida, the University of Southern California and the National MagLab, involves DNA sequencing. The team sequences the genomes of tumors removed from human patients, implants those tumors in mice, treats the rodents with Agyare’s nanoparticles (loaded with drug and contrast agent), then observes the varying results using MRI and other tools.
"We want to see how the tumors with different genetic makeups are forming and how they respond to tumor suppression," said Agyare.
What the team learns may help physicians in the future better design and adapt treatments for individual patients based on the genetics of their specific cases.


Likai Song

Edward Agyare
Track Closely
It's a big victory when a drug connects with its target, but that doesn't guarantee doctors will win the cancer war. Magnetic fields, once again, are helping them master the long game.
Duane Mitchell, a physician and immunologist at the University of Florida, studies immunotherapies such as adoptive cell transfer. In ACT, researchers take immune cells from a patient, modify them to enhance their ability to fight cancer, and then deliver those cells back to the patient.
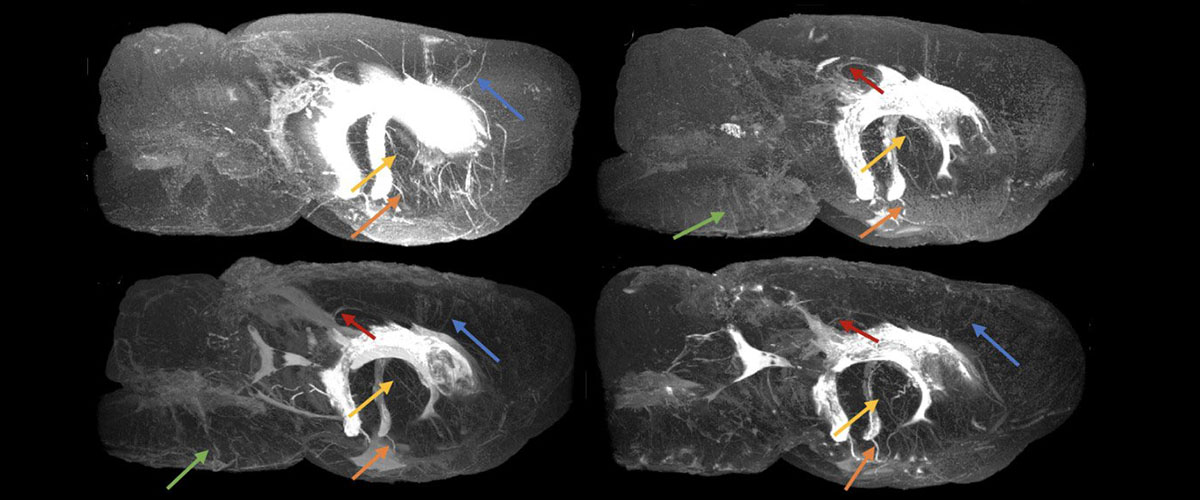
Specifically, he and his colleagues have used iron oxide-loaded nanoparticles to deliver dendritic cell vaccines (a type of ACT) to mice bearing invasive melanoma and brain tumors. By packaging the vaccines with MRI-sensitive iron oxide, the researchers could trace them in a strong MRI machine at the National MagLab. After following the paths of these particles, they could tell, within just two days, if the mice were responding to the treatment.
"We've shown you can use MRI at very early time points after treatment to reliably predict successful treatment and differentiate responding from non-responding subjects," Mitchell explained.
This promising research has advanced to multi-institutional clinical trials. Mitchell and his colleagues have found that glioblastoma patients treated with dendritic cell vaccines were more likely to survive when the vaccines travelled successfully to a patient's lymph nodes, a part of the body's immune system where immune cells mature. The researchers' goal is to identify biomarkers that correlate to successful treatment and improve existing therapies.
In earlier clinical studies, Mitchell used radioactively labelled cells and SPECT/CT scans to follow the cells in the body. But MRI offers numerous advantages: It's more widely available, is better for following the fate of cells over longer periods of time, and doesn't involve potentially damaging radiation.
Sam Grant, a biomedical engineer at the National MagLab, uses a technique called chemical exchange saturation transfer (CEST) to study the progression of glioma. Glioma is a brain tumor that typically has a median survival time of about 15 months, even after a patient has received surgery and treatment.
CEST allows scientists to detect structures or processes in the body that traditional MRI can't visualize. MRI scanners are typically used to detect the hydrogen in the body's water; that information generates an image of structures in the body. In CEST, hydrogen atoms from specific molecules interchange with hydrogen atoms in free water within the body, highlighting the interactions of those target molecules in MRI scans.
Grant and his colleagues have been optimizing the technique for experiments in the MagLab's 21.1 tesla MRI magnet. Using CEST, they can identify metabolites, neurotransmitters and other molecules involved in tumor progression.
"Looking at the chemical exchange allows us to identify fairly unique patterns in the spectra that correspond to a tumor that is changing dynamically as it's growing," said Grant, who is also an associate professor at the FAMU-FSU College of Engineering.
Over the last several years, the researchers have discovered metabolites and lipids that specifically correspond to glioma progression in rat models. They believe these metabolites could one day serve as biomarkers to help detect glioma early.
Tumors can evolve to outsmart therapies. But it's still difficult to predict whether a tumor will become resistant. Here again, powerful magnets can help.
MagLab biophysicist Victor Schepkin uses the lab's 21.1-tesla MRI system to track sodium in tumors. After initiating chemotherapy in rodents with brain tumors, Schepkin performs brain scans that, thanks to the magnet's high field and special instrumentation, can detect how sodium concentration changes in the rodents' brains. If the drug works, the intracellular sodium in the dead cells will increase, a process detectable on MRI.
"People know that tumors may develop resistance to therapy," Schepkin said. "But in our experiments, we can actually see the changes in tumor resistance during therapy and quantify them."
In fact, Schepkin has discovered that the dose of chemotherapy can influence whether cancer cells evolve to resist it. Two separate, smaller doses of a drug slow a tumor's growth rate (but don't shrink it), and don't affect the tumor's resistance to chemo. On the other hand, one combined dose might initially shrink the tumor, but what remains becomes more resistant to therapy. So the larger, single dose actually leads to future tumor resistance.
His most exciting discovery, Schepkin said, is that sodium MRI can detect if a tumor is resistant even before the chemotherapy is initiated. The research suggests that, one day, physicians could use sodium MRI to individualize cancer therapy for their patients.
Tracking sodium using MRI requires a strong magnetic field, Schepkin said, because the sodium signal is several thousand times weaker than that of hydrogen, MRI's conventional target. Taking this technique into the clinic will require time, as high-field MRI for humans is still far in the future.
Still, magnetic fields, in the shape of different tools and techniques, are proving increasingly useful across a wide swath of cancer research.
"Despite its relatively recent development, MRI is considered among the top 10 medical discoveries of all time — up there with the thermometer, the stethoscope and eye glasses," said Lucio Frydman, chief scientist for chemistry and biology at the National MagLab and a professor in the Department of Chemical and Biological Physics at the Weizmann Institute of Sciences in Israel. "But in fact we have only scratched the surface of how magnetic resonance methods, and high-field magnetic resonance methods in particular, are poised to revolutionize the ways in which we see, better understand, treat and eventually defeat this hideous disease."


Duane Mitchell

Victor Schepkin
Read more
Find out more about the high-field research these scientists are you doing in the following publications.
Lissa Anderson
- Analysis of Monoclonal Antibodies in Human Serum as a Model for Clinical Monoclonal Gammopathy by Use of 21 Tesla FT-ICR Top-Down and Middle-Down MS/MS, J Am Soc Mass Spectrom. 2017
Edward Agyare
- Smart thermosensitive liposomes for effective solid tumor therapy and in vivo imaging, PLoS One. 2017
- Engineering theranostic nanovehicles capable of targeting cerebrovascular amyloid deposits, J Control Release. 2014
Sam Grant
- Brain investigations of rodent disease models by chemical exchange saturation transfer at 21.1T, NMR In Biomedicine 2018
Victor Schepkin
- Use of MRI, metabolomic, and genomic biomarkers to identify mechanisms of chemoresistance in glioma, CDR 2019
Written by Wudan Yan and Kristen Coyne, Illustrated by Caroline McNiel